GENERAL MEDICINE ONLINE BLENDED BIMONTHLY ASSIGNMENT 1
Name: Samirishetty Manasa
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3.What is the drug rationale in CVA?
2.Why haven't we done pericardiocenetis in this pateint?
2.AFTER ADMISSION
iii)Glimi - Glimepiride + Metformin
Roll.no: 119
8th Semester
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link to the assignment :
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the assignment based on my understanding and clinical knowledge of the cases.
Pulmonology :
A. Link to the Patient Details :-
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A : Timeline of Symptomatology in this Patient :-
- 20 years Ago ( January,2001) :- Patient had Shortness of breath which lasted for 1 week while she was working in a paddy fields. This First episode was relieved upon taking Medication.
- From (2002-2009) :- Similar episodes of SOB every year which lasted for 1 week occuring in January when patient worked in paddy fields. All of these episodes were relieved upon taking Medication.
- 12 years Ago (2009) :- Patient had another episode of SOB which lasted for 20 days and needed hospitalisation.
- Since 12years (2009-2021) :- Patient has been having an yearly episodes which have lasted for month again around January, which are of Grade 2.
- 8 years Ago (2013) :- Patient was diagnosed with Diabetes, when patient had seeked help for Polyuria and is being treated for it ever since.
- 5 years Ago (2016) :- Patient was treated for Anaemia with Iron injections.
- 1 month Ago ( April,2021) :- Patient had Generalized Weakness for which she was administered IV fluids (3 pints in 2 days) by a local RMP.
- 30 days Ago (17/04/2021) :- Patient had latest episode of SOB.
- 20 days Ago (27/04/2021) :- HRCT done outside which showed the signs of Bronchiectasis.
- 20 days Ago (27/04/2021) :- Patient was diagnosed with Hypertension and is being treated for the same.
- Since 15 days (02/05/2021) :- Patient has pedal edema upto the level of ankle (Pitting type).
- Since 15 days (02/05/2021) :- Patient developed Facial puffiness.
- Since 2 days (15/05/2021) :- Patient was having SOB even at rest ( Grade 4) which not relieved with nebulizers and also has Drowsiness and Decreased Urine output.
Anatomical location : Bronchi and the Bronchioles
Primary etiology : Inhalation of paddy dust and noxious gases from chulha.
The patient has been experiencing dyspnea while working in the paddy field . So, the paddy dust could be responsible for her symptom.
In chronic COPD, it can cause the right-sided heart failure. This occurs when low oxygen levels due to COPD cause a rise in blood pressure in the arteries of the lungs, a condition known as pulmonary hypertension.
2)What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A: Pharmacological interventions used for the patient :
i) INJ.AUGMENTIN - amoxicillin + clavulanic acid
- MOA : Amoxicillin binds to penicillin-binding proteins within the bacterial cell wall and inhibits bacterial cell wall synthesis. Clavulanic acid is a β-lactam, structurally related to penicillin, that may inactivate certain β-lactamase enzymes.
- Indication: To treat bacterial infections, shorten the course of the disease, prevent further deterioration of lung function, and prolong the period between exacerbations.
ii) TAB.AZITHROMYCIN
- MOA: Azithromycin prevents bacteria from growing by interfering with their protein synthesis. It binds to the 50S subunit of the bacterial ribosome, thus inhibiting translation of mRNA.
- Indication : To treat Acute exacerbations of COPD
iii) INJ.LASIX - Furosemide
- MOA: Furosemide, like other loop diuretics, acts by inhibiting the luminal Na-K-Cl co-transporter in the thick ascending limb of the loop of Henle, by binding to the chloride transport channel, thus causing sodium, chloride, and potassium loss in urine.
- Indication : To treat pedal edema
iv) TAB PANTOP
- MOA : In the gastric parietal cell of the stomach, pantoprazole covalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion. The covalent binding prevents acid secretion for up to 24 hours and longer.
- Indication : To treat the acidity caused by antibiotics
v) INJ.HYDROCORTISONE :
MOA : Hydrocortisone is as a Corticosteroid Hormone Receptor Agonist. It works by reducing inflammation (irritation and swelling) in the body.
vi) NEB. with IPRAVENT, BUDECORT
- MOA :Ipratropium is an acetylcholine antagonist via blockade of muscarinic cholinergic receptors. Blocking cholinergic receptors decreases the production of cyclic guanosine monophosphate (cGMP). This decrease in the lung airways will lead to decreased contraction of the smooth muscles. Budesonide is a potent topical anti-inflammatory agent. [19] It binds and activates glucocorticoid receptors (GR) in the effector cell (e.g., bronchial) cytoplasm that allows the translocation of this budesonide-GR complex in the bronchi nucleus, which binds to both HDCA2 and CBP (HAT)
- Indication : To treat shortness of breath
vii) TAB PULMOCLEAR
- MOA : Acebrophylline is a compound which has been found to act both as a mucoregulating and a bronchodilating drug, works by relaxing the airways.
- Indication :Treatment of COPD
Non-pharmacological interventions :
i) Head end elevation : The elevation of the head of bed (HOB) to a semi-recumbent position is associated with a decreased incidence of aspiration and ventilator-associated pneumonia (VAP). It also can increase the possibility of more homogeneous alveolar ventilation and possibly reduce the risk of lung injury caused by mechanical ventilation
ii) BiPAP: BiPAP therapy targets dysfunctional breathing patterns. By having a custom air pressure for when you inhale and a second custom air pressure when you exhale, the machine is able to provide relief to your overworked lungs and chest wall muscles.
Indication : To treat COPD
iii) Chest physiotherapy : Chest physiotherapy involves a number of physical techniques to help remove excess mucus from respiratory passages and improve breathing. The goal is to help patients breathe more freely and get more oxygen through the blood stream into all parts of the body.
3) What could be the causes for her current acute exacerbation?
A : The most common cause of an exacerbation is infection in the lungs or airways (breathing tubes).
• This infection is often from a virus, but it may also be caused by bacteria or less common types of organisms.
• In this Patient, it could be the bacterial Infection which was responsible for her Acute Exacerbation of COPD (Mycobacterium tuberculosis )
4. Could the ATT have affected her symptoms? If so how?
A: The ATT might have resulted in Acute Kidney Injury.
According to the history the patient started developing pedal edema and facial puffiness a few days after starting on ATT.
As facial puffiness and pedal edema are both signs of renal dysfunction it is possible that some of her symptoms are due AKI as a consequence of adverse reaction to ATT.
5) What could be the causes for her electrolyte imbalance?
A: Chronic hypoxia and hypercapnia secondary to the underlying pulmonary illness, heart failure or renal insufficiency, use of diuretics, SIADH, hypokalemia attributed to steroids bronchodilators, malnutrition, and poor intake of food during acute exacerbations are common contributing factors for Hyponatremia in Chronic Obstructive pulmonary disease.
• Respiratory Acidosis occurs when breathing out does not get rid of enough CO2. The increased CO2 that remains results in an acidic state. This can occur as a result of respiratory problems, such as COPD.
• Respiratory acidosis with metabolic alkalosis (due to renal compensation) in AECOPD patients with chronic hypercapnia is the usual cause of Hypochloremia in the patiens.
Common causes of deranged serum sodium levels include hyperglycemia,
use of thiazides or nonsteroidal anti-inflammatory drugs, congestive cardiac failure, chronic renal failure, and low dietary salt intake.19 Common causes
of hypokalemia include diarrhea, laxative abuse, vomiting, certain diuretics, drugs like insulin, β2 agonists, and theophylline.
Thus, COPD patients are predisposed to electrolyte imbalance.
In turn electrolyte imbalance can cause respiratory muscle weakness, cardiac arrhythmia, low cardiac output, etc.
NEUROLOGY:
A.Link to patient details:
https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A: Timeline of Symptomatology in this Patient :-
- 12 years ago: Started drinking alcohol
- 2 years ago: Diagnosed with Diabetes Mellitus, prescribed oral hypoglycemics
- 1 year ago: Has an episode of seizures
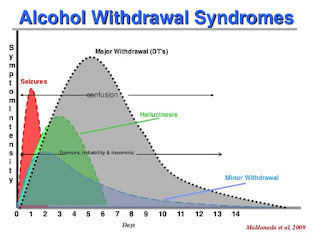
- 4months ago: Has another seizure episode (most likely GTCS)- after he stops taking alcohol for a day
- 11/5/21: Last alcohol intake, around 1 bottle. Has body aches that night
- 11/5/21: Decreased food intake. Starts talking and laughing to himself. Unable to lift himself off the bed. Goes to an RMP the same day- is prescribed IV fluids and asked to visit a hospital
- 15/5/21: Is admitted to a hospital for alcohol withdrawal symptoms, and is treated for the same.
Anatomical localisation: the brain in the hippocampus and frontal lobe.
Primary etiology : Chronic Alcoholic
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A.Pharmacological interventions used for the patient :
i) IVF NS and RL @150ml/hr
- MOA: replinishes the hydration of the body
- Indication: For dehydration.
ii) Thiamine
- MOA: thiamine diphosphate is a coenzyme in carbohydrate metabolism
- Indications: deficiency, wernicke's encephalopathy, beri beri.
iii) Inj. Lorazepam
- MOA: facilitate s GABA action and causes CNS depression.
- Indication: Used to sedate Patient
iv) T. Pregabalin 75mg/PO/ BD
- MOA: Acts by releasing GABA
- Indications: seizures
- Efficacy: Newer antiepileptic, good efficacy with fewer side effects
v) Inj. HAI S.C.- premeal
- MOA: Short- acting insulin
- Indications: Diabetes Mellitus
- Ef
vi) GRBS 6th hourly, premeal: 8am, 2pm, 8pm,2am
vii) Lactulose 30ml/PO/BD
For rehydration.
viii) Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
ix) Syp Potchlor 10ml in one glass water/PO/BD
- MOA: Potassium to increase serum K levels
- Indications: in hypokalemia
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
A. It could be because of something called kindling where repeated attempts at detoxification lead to increase in the severity of the symptoms of alcohol withdrawal.
This kindling in synergy to chronic alcohol use causes downregulation of GABA receptors and increased seizures.
4) What is the reason for giving thiamine in this patient?
A. A possible differential for this patients condition is Wernicke korsakoff syndrome which occurs due to vit. B1 deficiency, so in order to account for the possible differential thiamine is given.
5) What is the probable reason for kidney injury in this patient?
A. The renal injury is probably due to prerenal AKI with tubular necrosis. The AKI was probably caused due to dehydration. This can be said based on the increased s. Creatinine urea and FENa
6) What is the probable cause for the normocytic anemia?
A. The probable causes include:
- Decreased erythropoietin due to renal injury
- Hemolytic anemia
- Chronic blood loss from foot ulcer.
- Early VitB12 defeciency.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
A. Alcoholism can lead to peripheral neuropathy that can lead to nonhealing foot ulcers. Diabetes delays the wound healing leading to persistent foot ulcer.
B. Link to patient details:
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Timeline of Symptomatology in this Patient :-
- 7 days back- Patient gave a history of giddiness that started around 7 in the morning; subsided upon taking rest; associated with one episode of vomiting
- 4 days back- Patient consumed alcohol; He developed giddiness that was sudden onset, continuous and gradually progressive. It increased on standing and while walking.
- H/O postural instability- falls while walking
- Associated with bilateral hearing loss, aural fullness, presence of tinnitus
- Associated vomiting- 2-3 episodes per day, non projectile, non bilious without food particles
- Present day of admission- Slurring of speech, deviation of mouth that got resolved the same day
Anatomical location:- There is a presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology:- Ataxia is the lack of muscle control or co-ordination of voluntary movements, such as walking or picking up objects. This is usually a result of damage to the cerebellum (part of the brain that controls muscle co-ordination)
Many conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain medications eg. Barbituates, stroke, tumours, cerebral palsy, brain degeneration etc.
In this case, the patient has hypertension for which he has been prescribed medication that he has not taken. Stroke due to an infarct can be caused by blockade or bleeding in the brain due to which blood supply to the brain is decreased, depriving it of essential oxygen and nutrients. This process could’ve caused the infarct formation in the cerebellar region of the brain, thus causing cerebellar ataxia.
A. Pharmacological interventions used for the patient :
i) Tab Vertin 8mg- This is betahistine; It is an anti- vertigo medication
- MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
- Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
ii) Tab Zofer 4mg- This is ondanseteron; It is an anti emetic
- MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
- Indications- Used to control the episodes of vomiting and nausea in this patient.
iii) Tab Ecosprin 75mg- This is aspirin; It is an NSAID
- MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis
- Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
iv) Tab Atorvostatin 40mg- This is a statin
- MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
- Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
v) Clopidogrel 75mg- It is an antiplatelet medication
- MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
- Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting
vi) Thiamine- It is vitamin B1
- MOA- The patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
- Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
vii) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
3) Did the patients history of denovo hypertension contribute to his current condition?
A.A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelial dysfunction in this case. High BP can also promote cerebral small vessel disease. All these factors contribute to eventually lead to stroke.
4)Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic stroke?
A. Meta analysis of the relation between alcohol consumption and increased risk of stroke has mainly weighed in to the formation of two types- ischaemic and haemorrhagic stroke.
Ischaemic stroke- this is more common. This Is caused by a blood clot blocking the flow of blood and preventing oxygen from reaching the brain
Haemorrhagic stroke- occurs when an aneurysm bursts or when a weakened blood vessel leaks, thus causing cerebral hemorrhage
Alcoholics with mild and moderate drinking . the risk of ischaemic stroke decreases due to decreased level of fibrinogen which helps in the formation of blood clots. However, heavy alcohol intake is associated with impaired fibrinolysis, increased platelet activation and increased BP and heart rate.
Thus, the history of alcoholism, coupled with his hypertension definitely could be a causative factor of his current condition.
C) Link to patient details:
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A.Timeline of Symptomatology in this Patient :-
- 10 years ago - Paralysis of Right and Left upper and lower limbs.
- 1 year ago - Right and Left paresis
- 8 months ago - B/L pedal edema since then
- 7 months ago - Blood Infection
- 6 days ago - Pain radiating along left limb, more during palpitations
- 5 days ago - Dyspnea (NYHA grade 3) during palpitations, chest pain and chest heaviness
Anatomical location:- HEART
Etiology:- Palpitations, chest pain and SOB is HYPOKALEMIA
fforadiating pain of left upper limb is CERIVAL SPONDYLOSIS.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A. Risk factors for hypokalemia are female gender, heart failure, hypertension, alcoholism, diarrhea, eating disorders, and low body mass index.
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A. ECG changes in Hypokalemia -
- Mild Hypokalemia - Flattening and inversion of T waves.
- Moderate Hypokalemia - QT interval prolongation, visible U wave and mild ST depression.
- Severe Hypokalemia - Arrhythmias such as Torsades de points and ventricular tachycardia.
D)Link to patient details:
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
Questions:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
A.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason.
A.First the pt. did not have LOC which might mean the pt. has focal seizer which could most commonly can be simple partial A/K/A focal seizers without impairment of awareness that is without LOC. Then the pt. has developed generalized tonic clonic seizers which is usually associated with LOC.
E) Link to patient details:
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Questions:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
A.Since the patient is an alcoholic he might gave had an episode of fall which could have caused cerebellar injury.
Cerebellar damage is the most common cause of Ataxia. Seeing that the patient has a history of frequent falls. he might have injured his cerebellum during one of his falls.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
A.The patient has minor unattended head injuries due to his frequent falls.During the course of time the minor hemorrhages if present should have been cured on their own. Since the patient is a chronic alcoholic, the process of healing would have hindered and further contributing to its growth further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes.
F) Link to patient details:
http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
A.No , the history of RTA has no role in patient's current condition. Alcohol abuse and emotional stress could have led to his current scenario.
2.What are warning signs of CVA?
A.
1)GENERAL SUPPORTIVE CARE -
a. Oxygenation - In order to prevent hypoxia and worsening of neurological injury during periods of acute cerebral ischemia, maintaining adequate tissue oxygenation is important.
Supplemental oxygen - if hypoxia or desaturation is present.
Endotracheal intubation - if there is decreased consciousness.
b. Anti-hypertensives - Many patients may have elevated blood pressure in the first 24-48 hours.
I.V - Nicardipine or labetalol for adequate control of BP.
Oral - Labetalol or lisinopril for more sustained BP lowering.
c. Insulin - Hypoglycemia can cause focal neurologic signs that mimic stroke and can itself lead to brain injury. Subcutaneous Insulin is administered to keep glucose > 180 mg/dl.
d. Antipyretics - Increased body temperature has been associated with poor neurologic outcome due to increased metabolic demands, enhanced release of NT and increased free radical production. Maintaining normothermia might improve the prognosis of the patient. It is indicated if Temp > 37.5 C.
2)TREATMENT -
a.Thrombolysis -
I.V Alteplase is the only FDA approved medical therapy for treatment of patients with acute ischemic stroke. Tenecteplase, steptokinase, desmoteplase are other drugs available.
b.Device therapies - Mechanical thrombectomy delivered endovascularly is another option for clot removal, either as an adjunct to thrombolysis or for patients who are ineligible for IV Alteplase.
c.Anticoagulants -
d.Antiplatelet -
4. Does alcohol has any role in his attack?
A.Alcohol increases the risk of hemorrhagic stroke.
A hemorrhagic stroke occurs either when an aneurysm bursts, or a weakened blood vessel leaks. The result is bleeding either inside the brain, causing an intracerebral hemorrhage, or, less commonly, bleeding between the brain and the tissue covering it, causing a so-called subarachnoid hemorrhage.
The adverse effect of alcohol consumption on blood pressure – a major risk factor for stroke – may increase the risk of hemorrhagic stroke .
Liver damage due to excessive alcohol can stop the liver from making substances that help your blood to clot. This can increase your risk of having a stroke caused by bleeding in your brain.
5.Does his lipid profile has any role for his attack?
A.The lipid profile of the patient doesn't have any role as lipid profile is normal to cause attack.
G) Link to patient details:
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
Questions:
1)What is myelopathy hand ?
A.The “myelopathy hand” in cervical spondylosis includes findings of localised wasting and weakness of the extrinsic and intrinsic muscles of the hand.
2)What is finger escape ?
A.The finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign" or Wartenberg's sign . Upper motor neuron disorders of the cerebral cortex such as mild hemiplegic stroke or hemiplegic migraine where the same clinical finding has been called the "digiti quinti sign".
A.Hoffmann's reflex (Hoffmann's sign, sometimes simply " Hoffmann's ", also finger flexor reflex) is a neurological examination finding elicited by a reflex test which can help verify the presence or absence of issues arising from the corticospinal tract. It is named after neurologist Johann Hoffmann.
H) Link to patient details:
Questions:
1) What can be the cause of her condition ?
A.It might be cortical venous thrombosis according to the the results of imaging.
2) what are the risk factors for cortical vein thrombosis?
A.Infections:
1.meningitis, otitis,mastoiditis
2.prothrombotic states:
3.pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,hormone replacement therapy.
Mechanical:
1.head trauma,lumbar puncture
2.inflammatory:
3.sle,sarcoidosis,inflammatory bowel disease.
4.malignancy.
5.dehydration
6.nephrotic syndrome
Drugs:
1.Oral contraceptives,steroids,Inhibitors of angiogenesis
2.Chemotherapy:Cyclosporine and l asparginase
Hematological:
1.Myeloproliferative Malignancies
2.Primary and secondary polycythemia
Intracranial :
1.Dural fistula,
2.venous anomalies
Vasculitis:
1.Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
A. Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
A.Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor Xa.
CARDIOLOGY:
A) Link to patient details:
https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html
Questions:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
A.Aortic dissection and post-infarction rupture of the free wall are contraindications to needle pericardiocentesis (surgical tamponade) due to the potential risk of aggravating the dissection or myocardial rupture via rapid pericardial decompression and restoration of systemic arterial pressure.
3.What are the risk factors for development of heart failure in the patient?
A.The patient is old, and has a history of smoking and is also a known case of hypertension. These could've led to the development of heart failure in this patient.
4.What could be the cause for hypotension in this patient?
A.Among the heart conditions that can lead to low blood pressure are an abnormally low heart rate (bradycardia), problems with heart valves, heart attack and heart failure. Your heart may not be able to circulate enough blood to meet your body's needs.
B) Link to patient details:
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html.
Questions:
1.What are the possible causes for heart failure in this patient?
A.Obesity, DM, HTN and alcohol consumption contribute as risk factors for heart failure in this patient.
2.what is the reason for anaemia in this case?
A. Alcohol consumption, Chronic kidney disease, heart failure and truncal obesity are all associated with normocytic normochromic anaemia as seen in this patient.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
A.Blebs and non healing ulcers are caused due to his diabetes. Ulcers in people with diabetes are most commonly caused by:
- poor circulation
- high blood sugar (hyperglycaemia)
- nerve damage
- Irritated or wounded feet
4. What sequence of stages of diabetes has been noted in this patient?
A.Stage 1: Insulin resistance
Stage 2: Pre-diabetic
Stage 3: Diabetes type 2
Stage 4: Microvascular complications
C) Link to patient details:
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A.Timeline of Symptomatology in this Patient :
1.BEFORE VISITING THE HOSPITAL
- 10yrs ago - Operation for Hernia
- Since 2-3 yrs - Facial puffiness
- 1 yr ago - SOB grade I
- 1yr ago - was diagnosed with Hypertension
- Since 2 days - SOB which progressed from Grade II to Grade IV.
- Since 2 days - Decreased urine output.
- Since 1 day - Anuria
3.ON INVESTIGATION
- CT scan - Showed dilated pulmonary vessels and thrombi in the atria.
- 2D Echo - Showed LV dysfunction.
Anatomical location:- Atria (SA node)
Etiology:- Hypertension
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A.Pharmacological interventions:-
i)Digoxin - It is a cardiac glycoside
- MOA - It increases intracellular sodium that will cause an influx of calcium in the heart and cause an increase in contractility. It is vagomimetic.
- Indications - Heart failure and arrhythmias.
ii)Carvediol - It is a beta-blocker.
- MOA - It blocks the beta receptors and lowers the heart rate, blood pressure and strain on the heart.
- Indications - Hypertension, heart failure, LV dysfunction with MI.
iii)Heparin - It is an anti-coagulant
- MOA - It produces its major anticoagulant effect by inactivating thrombin and activated factor X through an antithrombin dependent mechanism. By inactivating thrombin, heparin not only prevents fibrin formation but also inhibits thrombin induced activation of platelets and of factors V and VIII.
- Indications - Prophylaxis and treatment of venous thromboembolism and pulmonary embolism; Atrial fibrillation with embolization ; chronic consumptive coagulopathies.
iv) Acitrom - It is an Oral anti-coagulant
- MOA - It inhibits the reduction of Vitamin K by Vitamin K reductase. This prevents carboxylation of Vitamin K dependent clotting factors, II, VII, IX, X and interferes with coagulation.
- Indications - Thromboembolic diseases such as DVT, Coronary occlusion
v)Cardivas - It is an adrenergic blocker
- MOA - Reversibly binds to beta adrenergic receptors on cardiac myocytes. Inhibition of these receptors prevent a response to the sympathetic nervous system, leading to decreased Heart rate and contractility
- Indications - Hypertension, Angina and heart failure.
vi)Dytor - It is a diuretic. Contains Torsemide + Spironolactone
- MOA - Through its action in antogonizing effect of Aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
- Indications - Edema, Hypertension.
vii)Pan D - It is a Proton pump inhibitor
- MOA - Inhibits the final step in gastric acid production. In the gastric parietal cell of stomach, it binds to H+/K+ ATP pump to inhibit gastric acid and basal acid secretion
- Indications - Heavy bloating, gas, heart burn, indigestion, GERD.
viii) Taxim - It is a cephalosporin antibiotic.
- MOA - It is bactericidal through inhibition of cell wall synthesis
- Indications - Treatment of infections of throat, airway and urinary tract ; Typhoid fever.
ix)Thiamine - It is Vitamin B1.
- MOA - Rapid restoration of Thiamine level
- Indications - Wernicke's encephalopathy, infantile beriberi etc.
x) Inj. HAI - It is a short acting insulin.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
- The patient has Cardiorenal syndrome 4.
4) What are the risk factors for atherosclerosis in this patient?
A.- The risk factors for atherosclerosis are hypertension, high cholesterol and triglyceride, DM-1, obesity, physical inactivity, smoking, high saturated fat diet.
This patient has three risk factors: Hypertension, physical inactivity and obesity.
5) Why was the patient asked to get those APTT, INR tests for review?
A.The patient was on Anticoagulants. So to predict the occurrence of CVA and ischemic attacks, the patient is advised to get these tests.
D) Link to patient details:
https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Timeline of symptomatology in this patient:-
- Diabetes since 12 years - on medication
- Heart burn like episodes since an year- relieved without medication.
- 7 months ago- Diagnosed with pulmonary TB, completed full course of treatment, presently sputum negative.
- Hypertension since 6 months - on medication
- Shortness of breath since half an hour-SOB even at rest
Anatomical location:- Coronary circulation
Etiology:-
- Smoking.
- High blood pressure.
- High blood cholesterol.
- Diabetes.
- Physical inactivity.
- Being overweight or obese.
- A family history of chest pain, heart disease or stroke.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A.Pharmacological interventions:-
i) Met XL - It is a Beta-blocker
ii)Telma - It is an Angiotensin receptor blocker
- MOA - It blocks Beta receptors and slow down heart rate, and makes pumping more efficient.
- Indications - Hypertension, Angina, arrhythmias, migraine.
ii)Telma - It is an Angiotensin receptor blocker
- MOA - It binds to angiotensin II type 1 receptors with high affinity, causing inhibition of action of Angiotensin II on vascular smooth muscle leading to reduction in arterial blood pressure.
- Indications - HTN, diabetic nephropathy, CHF.
iii)Glimi - Glimepiride + Metformin
- MOA - The primary mechanism of action of Glimepiride is stimulating release of insulin from functioning pancreatic beta cells. Metformin reduces insulin resistance.
- Indications - DM 2
3) What are the indications and contraindications for PCI?
A.Indications -
- Stable angina
- Unstable angina
- STEMI
- NSTE - ACS
- Anginal equivalent
Contraindications -
- Chronic kidney disease
- Hyper coagulable state
- Intolerance to oral antiplatelet therapy.
- Chronic total occlusion of SVG.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
A.PCI being performed in a patient who doesn't need it might lead to unnecessary complications and extra expenditure burden on the patient.
Research on over testing and over treatment is importance in our present health care systems because there is development of resistance in the microorganisms to the effective drugs being produced.
Over treatment might also make our body's immune system to be dependent on the medication
E) Link to patient details:
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A.Timeline Symptomatology in this patient:-
- Since 8 years - DM type 2
- 5 days ago - received COVISHIELD vaccine
- Since 3 days - Chest pain
- Since morning - Giddiness and Sweating
Anatomical location:- Heart
Etiology:- Uncontrolled DM
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A. Pharmacological interventions:-
i)TAB. ASPIRIN
- MOA - It inhibits COX-1 and COX-2 to decrease the Prostaglandin and thromboxane synthesis.
- Indications - used as anti platelet drugs to prevent clot formation and stroke.
ii) TAB. ATORVASTATIN
- MOA - It is a HMG CoA reductase inhibitor and thus inhibits the cholesterol synthesis. It decreases VLDL, LDL in the blood, cholesterol synthesis. It increases LDL receptors in the liver and increases LDL uptake and degeneration. Thus decreasing LDL levels in the plasma.
- Indications - Primary hyperlipidemias and prevention of stroke.
iii) TAB. CLOPIDOGREL
- MOA - It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
- Indications - To decrease risk of heart disease and prevent stroke.
iv) Inj. HAI - It is a short acting insulin.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
A. PTCA after 12 hours is acceptable but after 3 days is not correct and can lead to complications.
Gastroenterology (& Pulmonology)
A) Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A. Timeline of symptomatology in this patient:-
- 5years ago- developed pain abdomen and vomiting
- 1 week ago- developed pain abdomen
- 4days ago- developed fever , constipation and burning micturition.
Anatomical location:- Pancreas
Etiology:- chronic alcohol consumption
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A. Ulinastatin plus octreotide can significantly improve the serum and clinical parameters and reduce the incidence of complications in severe acute pancreatitis patients. And it is worthy of wider popularization.
Approach to the patient:
1) Fluid Resuscitation
2) Nutrition
3) Pain management - Opioids
4) Antibiotics
5) Endoscopy
B) Link to patient details:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
A.PLEURAL EFFUSION
Two main causes of pleural effusion are:
• Transdiaphragmatic lymphatic blockage leading to increased permeability.
• Pancreatico-pleural fistulae secondary to leak and disruption of the pancreatic duct or pseudocyst caused by an episode of acute pancreatitis.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
A.Elevated cortisol
Damaged pancreatic beta cells leading to downregulation of insulin
Elevated levels of corticosteroids.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
A. 1.LFT are increased due to hepatocyte injury
- If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage.
- elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
2.The reasons for a classical 2:1 excess of serum AST activity compared to serum ALT activity in alcoholic hepatitis have been attributed to
(i) decreased ALT activity most likely due to B6 depletion in the livers of alcoholics
(ii) mitochondrial damage
4) What is the line of treatment in this patient?
Plan of action and Treatment:
A.
1. Investigations:
- ✓ 24 hour urinary protein
- ✓ Fasting and Post prandial Blood glucose
- ✓ HbA1c
- ✓ USG guided pleural tapping
2. Treatment:
- IVF: 125 mL/hr
- Inj PAN 40mg i.v OD
- Inj ZOFER 4mg i.v sos
- Inj Tramadol 1 amp in 100 mL NS, i.v sos
- Tab Dolo 650mg sos
- GRBS charting 6th hourly
- BP charting 8th hourly
C) Link to patient details:
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
Questions :-
1) what is the most probable diagnosis in this patient?
A. Abdominal hemorrhage
Differential diagnosis:
- Ruptured liver abscess
- Intraperitoneal hematoma
- Free fluid in sub diaphragmatic space
2) What was the cause of her death?
A.She undergone laporomy surgery .May be patient died due to complications of surgery like hemorrhage or infection.
3) Does her NSAID abuse have something to do with her condition? How?
A.Yes , NSAID may caused hepatotoxicity .
It might have lead to renal dysfunction like decreased gfr, and acute renal failure.
Nephrology (and Urology)
A) Link to patient details:
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
1. What could be the reason for his SOB ?
A.A. Metabolic acidosis could be the possible reason for his SOB.The respiratory center in the brainstem is stimulated, and hyperventilation develops in an effort to compensate for the acidosis. As a result, patients may report varying degrees of dyspnea.
2. Why does he have intermittent episodes of drowsiness ?
A. The most probable cause for drowsiness in this patient could be hyponatremia which occurred due to the use of diuretics
3. Why did he complaint of fleshy mass like passage in his urine?
A. The fleshy mass like passage in his urine was due to pyuria.
4. What are the complications of TURP that he may have had?
A. Complications of TURP :
- Bladder injury.
- Bleeding.
- Blood in the urine after surgery.
- Electrolyte abnormalities.
- Infection.
- Loss of erections.
- Painful or difficult urination.
- Retrograde ejaculation (when ejaculate goes into the bladder and not out the penis)
B) Link to patient details:
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?A.One possible Provisional diagnosis of this patient is ADHD (Attention deficit/Hyperactive disorder).
Symptoms may start before the age of 12 and include inattention and hyper active impulsive behavior.
Inattention -
- They have trouble to stay focused in tasks or play.
- They appear not to listen even when spoken directly.
- They are easily distracted.
- They avoid or dislike tasks that require mental effort.
- Have difficulty sitting in one place and are always on the run.
- Fidget with their hands or legs.
- Talk too much
- Have difficulty waiting for their turn.
- Academic difficulties are frequent as are problems with relationships.
2. Why doesn't the child have the excessive urge of urination at night time ?
A.It maybe Psychosomatic. The child has the urge to urinate in the morning due to stress or mental conflict. During sleep, the kid is free of stress and may not have the urge to urinate excessively.
3. How would you want to manage the patient to relieve him of his symptoms?
A.The only management is reassurance to the kid and his relaxation by reducing stress. The problem will resolve overtime (most commonly by the time he reaches 10yrs).
There are a variety of psychotherapeutic approaches employed by psychologists and psychiatrists; the one used depends on the patient and the patient's symptoms. The approaches include psychotherapy, cognitive-behavior therapy, support groups, parent training, meditation, and social skills training.
Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) :
A) Link to patient details:
https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
A.CLINICAL HISTORY:
- Cough on taking foods and liquids which was initially non productive then associated with sputum which is white in colour and non foul smelling.
- Difficult in swallowing since 2 months with solids and liquids. Patient is on RT feeding.
- History of weight loss and SOB
- One episode of vomiting
- Fever episodes
PHYSICAL FINDINGS:
- Poorly built and malnourished
- Respiratory system examination: Wheeze present in bilateral mammary areas.
- Neck examination: laryngeal crepitus- positive
2.What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
A. The chances are very less.
PREVENTION:
* The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
* Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
* Two prospective randomized studies are evaluating prednisone and meloxicam for the prevention of paradoxical TB IRIS.
Infectious disease and Hepatology:
A.Link to patient details:
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?
A.Local indigenously prepared alcohol do cause the liver abscess mostly contributing to the amoebic liver abscess than the pyogenic liver abscess due to the harmful effects of alcohol on liver.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
A.
3. Is liver abscess more common in right lobe ?
A. Liver abscess in common in right lobe as it receives more blood supply than the left lobe. Since the liver receives its blood circulation from the systemic and portal circulations, it is more susceptible to getting infections and abscesses from the bloodstream.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
A.1) If the abscess is large ( 5cm or more) because it has more chances to rupture.
2) If the abscess is present in left lobe as it may increase the chance of peritoneal leak and pericardial leak.
3) If the abscess is not responding to the drugs for 7 or more days .
B) Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
QUESTIONS:
1.Cause of liver abcess in this patient ?
A.The cause of the liver abscess id due to ENTAMOEBA HISTOLYTICA.
2.How do you approach this patient ?
A.We treat for pyogenic and amoebic liver abcess , we cover both bacterial causes with broad spectrum antibiotics and also amoebic causes mostly with metronidazole.
Then we administer patient with analgesic and antipyretic such as tab.dolo 650mg & tab.Ultracet , to relieve pain and fever.
*Abcess may get ruptured if untreated and cause peritonitis and shock*
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
A.Beacuse we cant differentiate whether the abcess is because of bacterial infection or amoebic infecation.
So we cover both bacterial causes with broad spectrum antibiotics and also amoebic causes mostly with metronidazole.
4) Is there a way to confirm the definitive diagnosis in this patient?
A.The diagnosis of an amebic liver abscess is made through a combination of characteristic findings on imaging and serologic testing. On imaging, there is a cystic intrahepatic cavity that is usually indistinguishable from other causes of liver abscesses. The majority of amebic liver abscesses are solitary lesions, although there can occasionally be multiple lesions, and they are more often found in the right lobe than the left. On ultrasound, the lesion is a round, well-defined hypoechoic mass . After healing, the periphery of the abscess may calcify and form a round, thin rim.
Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) :
A.Link to patient details:
http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A.Timeline of symptomatology in this patient :
1. 3years ago- diagnosed with hypertension
2. 21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
3. 18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
4. 11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
5. 4 days ago-
- patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb.
- towards the evening patient periorbital oedema progressed.
- serous discharge from the left eye that was blood tinged.
- was diagnosed with diabetes mellitus.
He was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then. This resulted in poorly controlled blood sugar levels.
The patient was diagnosed with acute oro rhino orbital mucormycosis . rhino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes the fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA
Anatomical location: Eye, nasal cavity
Etiology: Diabetes.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A. Amphotericin B has proven efficacy in the treatment of mucormycosis. At the present time, the liposomal formulation (AmBisome) is the drug of choice based on efficacy and safety data.
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
A.Mucormycosis is may be being triggered by the use of steroids, a life-saving treatment for severe and critically ill Covid-19 patients. Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing.
Infectious Disease (Covid 19):
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
Please check out the thesis log here for the example of a blogged master chart https://vamsikrishna1996.blogspot.com/2020/10/thesis.html and please get in touch with Dr Sai Charan PGY1 who is liasing between us and the MRD for this project where we hope this data can allow us to get some clues on predicting the factors driving recovery from covid 19.
10) Medical Education:
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research. A sample answer to this last assignment around sharing your experience log of the month can be seen in the link below but while this is by a student onsite in hospital and not locked down at home we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home: https://onedrive.live.com/view.aspx?resid=4EF578BAE67BA469!4180&ithint=file%2cdocx&authkey=!AOy7BpRTn42DBMo
This telemedicine has been a great opportunity to learn about various conditions in this current scenario of COVID. This has provided us with a platform to study and understand various clinical scenarios. The discussions around these cases have given us an outlook on the various differential diagnosis to the symptoms of the patients. Numerous research papers shared on various topics have given us an insight about the logistics and details on the cases.



























Comments
Post a Comment