FINAL PRACTICAL EXAM LONG CASE
This is an online E-Log book to discuss our patient's de-identified data shared after taking his/her/Guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve these patient's clinical problems with collective current best evidence-based inputs. This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
ROLL NO: 1701006162
A 75 years old female, resident of nalgonda, came to casualty on 9th June 2022 with
CHIEF COMPLAINTS:
Vomiting and giddiness since morning.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 6 years back then she had complaints of headache and generalised weakness, for which she visited hospital was diagnosed with type 2 diabetic mellitus and hypertension. She used medication for the same.( Glimepiride 1mg and metformin 500mg)
PAST HISTORY:
PERSONAL HISTORY:
- Diet:mixed
- Appetite: normal
- Sleep: adequate
- Bowel and bladder movements: regular
- Addictions:Consumes alcohol occasionally (90mL), smoked chutta for 10years, stopped 5 years back
- No history of allergies
FAMILY HISTORY:
GENERAL EXAMINATION:
SYSTEMIC EXAMINATION:
- Respiratory system: Normal vesicular breath sounds heard.
- CVS: S1 and S2 heard, no murmurs.
- CNS: no focal neural deficit
- Per Abdomen: soft, non tender, no abdominal mass.
INVESTIGATIONS:
- Random blood sugar: 164mg/dl
- Blood Urea: 26mg/fl
- Serum Creatinine: 1.0 mg/dl
- Electrolytes: Sodium - 139mEq/L Potassium- 3.3mEq/L. Chloride -98mEq/L
- Complete urine examination:
- Albumin: ++
- Sugar: ++++
- Pus cells: 3-6 /HPF
- Epithelial cells: 2-4 / HPF
- Red blood cell: NIL
- Casts: NIL
- Hemoglobin: 11.3mg/dl
- Total leucocyte count: 8900cell/cumm
- Neutrophils: 80
- Lymphocytes:13
- Eosinophils:02
- Monocytes:05
- Platelets: 2.67 lakhs/cumm
- RBC: 4.47million/cumm
- Total bilirubin: 0.74mg/dl
- Direct bilirubin: 0.18mg/dl
- Aspartate transaminase: 29IU/L
- Alkaline phosphate: 143IU/L
- Alanine transaminase: 11IU/L
- Total proteins: 7.7g/dl
- Albumin: 4.1g/dl
- A/G ratio: 1.16
- pH : 7.44
- pCO2 : 30.6mmHg
- pO2. :71.4mmHg
- HCO3:22.6mmol/L
- O2sat:93.8%
PROVISIONAL DIAGNOSIS:
TREATMENT:
- Intravenous fluids normal saline/ ringer lactate @100ml/hr
- Injection Human actrapid insulin I.V infusion @6ml/hr
- Inj. OPTINEURON 1 ampoule in 100ml NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
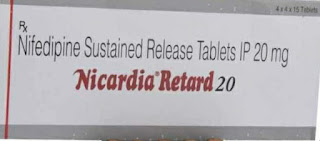
- Tab. NICARDIA 20mg PO/ STAT
- Monitor GRBS, PR, BP, RR CHARTING hourly
- Intravenous fluids NS 2 @ 100ML/hr
- Injection Human actrapid insulin I.V infusion @6ml/hr
- Inj. OPTINEURON 1 ampoule in 100ml NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab TELMA- AM (40/5) mg PO OD
- MONITORING GRBS,BP,PR, RR CHARTING
- Intravenous fluids NS 2 @ 75mL/hr
- Injection Human actrapid insuin 10/10/10 and NPH 8/-/8 ,strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS (IV)/ OD
- Inj. ZOFER 4mg IV/ TID
- Tab CINOD-T (40/10) mg PO OD
- MONITORING BP 2nd hourly charting











Comments
Post a Comment